
About Shingles
Welcome to the illuminate About Shingles page.
This page focuses on shingles, a common debilitating condition. Learn more about the symptoms, causes and importance of vaccination.
Adverse events reporting and prescribing information can be found at the bottom of the page.
Healthcare professionals have been consulted by GSK and received honorarium.

Shingles: More than just a rash
If you’ve seen shingles in your practice, you’ve probably seen how it can be a painful, debilitating disease that can lead to serious and long-lasting complications.1–3
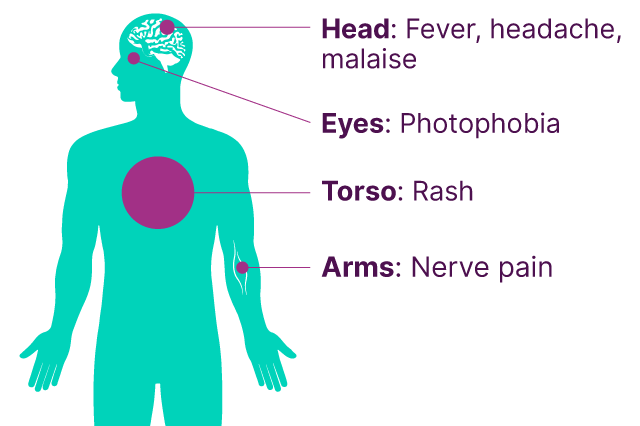
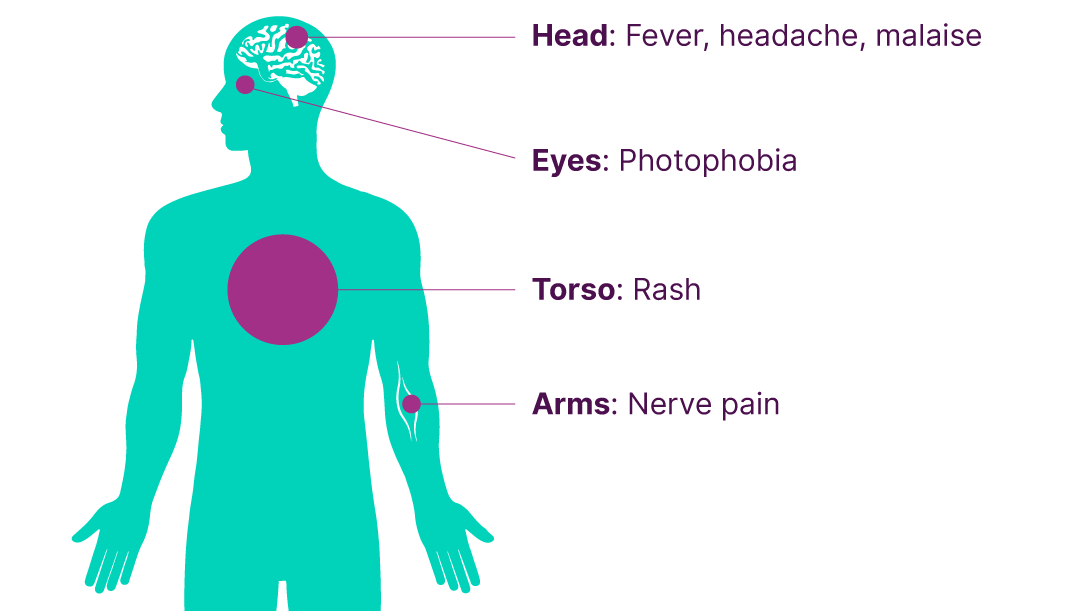
Many of us are familiar with the rashes or blisters we see on one side of the body with shingles, but symptoms can also include burning or shooting pains, itching, fever, fatigue, photophobia, malaise and headaches.2,4 It often starts with an unusual skin sensation and pain in the affected area, that is then followed by a rash of fluid-filled blisters.2
Shingles isn’t to be taken lightly though, even after the rash has resolved, shingles can still have long-term consequences. Between 10–20% of those affected by shingles over the age of 50 develop post-herpetic neuralgia (PHN). This is characterised by long-lasting nerve pain that can last for anywhere from 3 months to several years1 and lead to hospitalisation.2
Where can shingles occur?
The shingles rash often looks like a band or a stripe that wraps around one side of the patient’s body following the path of the affected nerve.5
However, shingles can occur anywhere on the body including the legs, arms, back, head, and eyes, each affecting the patient differently. In some cases, patients might experience symptoms that impact multiple places at once, for example, a rash could appear on your patient's body, but they might also experience photophobia in their eyes.4,5
Shingles causes
Most people in the UK have been infected with the chickenpox (varicella zoster) virus; in fact, people have a lifetime risk of infection of over 95%.2 This initial infection causes chickenpox in children, while the virus migrates to the dorsal root ganglia where it remains dormant. Reactivation of the dormant virus in adulthood causes shingles, with the risk and severity of it increasing with age.2,6
Prevalence and incidence of shingles
With so many people carrying the dormant varicella virus, it’s perhaps unsurprising that shingles is common. A quarter of all people develop shingles in their lifetime, with an overall annual incidence of between 1.85–3.9 cases per 1,000 people in the UK.7
While shingles can affect individuals of any age, it becomes much more common as people get older.1,2 In England and Wales, for those aged between 65–69, there are about 7.91 cases per 1,000 people,2 while for those aged 70–79 years it is likely to be even higher at around 7.90–8.80 cases per 1,000 people.2,7
The increased risk of shingles as we get older is thought to be due to our reducing immunity as we age. Patients that are severely immunocompromised also have an increased risk of developing shingles; these include people with primary or acquired immunodeficiency such as leukaemia or HIV/AIDS; people receiving immunosuppressive or immunomodulating therapy such as chemotherapy or immune-targeting monoclonal antibodies; or people with chronic immune-mediated inflammatory disease who are receiving or received immunosuppressive therapy such as moderate to high dose corticosteroids.2,8
Burden of shingles
The burden of shingles can go far beyond a painful rash; it can have an enormous impact on the quality of life of both patients and their caregivers. From sleeping, socialising, working and performing day-to-day chores, shingles has been shown to have a long-term impact on daily life.1
Shingles can also impact your clinical practice, with long-term complications resulting in patients repeatedly returning, draining your clinic’s time, resources and capacity.9,13
One of most debilitating complications associated with shingles is PHN, which affects 10–20% of patients aged 50 and over.1 Patients with PHN have constant or intermittent burning, stabbing, or sharp, shooting pains that limit daily living.9
Estimated percentage by age group of the population developing PHN in England and Wales in 2007
| Age group | Proportion developing PHN after 90 days |
|---|---|
| 60-64 years | 9% |
| 65-69 years | 11% |
| 70-74 years | 15% |
| 74-79 years | 20% |
| 80-84 years | 27% |
| 85+ years | 52% |
| Age group | 60-64 years | 65-69 years | 70-74 years | 74-79 years | 80-84 years | 85+ years |
|---|---|---|---|---|---|---|
| Proportion developing PHN after 90 days | 9% | 11% | 15% | 20% | 27% | 52% |
Adapted from DH Green Book ch 28a – Shingles (herpes zoster), 2021.2
PHN can also be tricky to treat; it does not respond well to painkillers such as paracetamol or ibuprofen, and may mean the patient has to go into hospital.10,11
Beyond PHN, other long-term complications have also been seen in patients with shingles. These include vasculitis, stroke, motor weakness, facial palsy and disseminated, ophthalmic, neurologic, and visceral involvement or disease.12
The importance of shingles vaccination
While this shingles programme rollout hasn't been as effective as other programmes such as the influenza vaccine, its importance shouldn't be overlooked.14 Even in those patients who do develop shingles despite having had the vaccine, the symptoms they experience are typically milder and last a shorter amount of time than patients who weren’t vaccinated.15 Increased uptake of the shingles vaccine resulted in reports of fewer GP appointments and hospitalisations required for shingles and PHN.13
The impact of shingles can be debilitating for patients, so it is important to remember that it can be routinely prevented through effective immunisation and the Shingles National Immunisation Programme. Given the current guidance for shingles, you and your peers are at the forefront of this opportunity to improve vaccine uptake and reduce the burden of shingles, while at the same time helping prevent a range of complications and reducing the need for appointments and hospitalisations.

Severely Immunocompromised individuals are at risk of severe disease - are you helping to protect them?
Discover tools and guidance on how to implement the Shingles National Immunisation Programme for your vulnerable severely immunocompromised patients, as defined in the Green Book Chapter 28a.
Severely Immunocompromised individualsFAQs on shingles from patients
The stages of shingles or progression of shingles can be broadly separated into three phases: pre-eruptive, acute exudative, and chronic.4
During the pre-eruptive stage, your patients may experience burning or pain on the skin at least 2 days before cutaneous eruptions. Non-cutaneous symptoms may include headaches, general malaise and photophobia, among others.4
In the acute exudative phase, your patients will develop painful lesions which burst, ulcerate and dry out. Pain is often severe, and responds poorly to non-steroidal pain medications. This phase may last approximately 2–4 weeks.4
Shingles is characterised as chronic if severe pain is present for 4 weeks or more post-infection. During this time, your patients can experience disabling pain, dysesthesia and paresthesia.4
People with active shingles lesions, particularly those who are immunocompromised, can transmit the varicella zoster virus to at-risk individuals, causing chickenpox. However, there is no evidence to suggest shingles can be acquired from chickenpox.2
Treatment is typically with the anti-viral shingles medication acyclovir. Less frequently used treatments may include valaciclovir or famciclovir.4 Treatment should be given within 72 hours of rash onset.1,16 Antivirals are ineffective and not recommended for PHN.17
Over-the-counter non-steroidal anti-inflammatory pain medications, such as ibuprofen, may also be suggested to ease pain.18
Advise your patients to:18
- Keep the rash clean and dry to reduce the risk of infection
- Wear loose-fitting clothing so that the fabric does not catch the skin
- Use calamine lotion to relieve the itching
Although uncommon, it is possible to have shingles more than once. But it is extremely rare to get it more than twice.18,19
References
- Johnson RW, et al. BMC Medicine. 2010;8:37.
- UKHSA Green Book Ch 28a. Shingles. 2024.
- Lukas K, et al. J Public Health. 2012;20:441–451.
- Patil A, et al. Viruses. 2022;14(2):192.
- MayoClinic. Shingles. Available at: https://www.mayoclinic.org/diseases-conditions/shingles/symptoms-causes/syc-20353054. Accessed March 2025.
- UKHSA Green Book. Ch 34. Varicella. 2024.
- NICE clinical knowledge summaries. Shingles. Prevalence, 2024. Available at: https://cks.nice.org.uk/topics/shingles/background-information/prevalence/. Accessed March 2025.
- Safonova E, et al. Respiratory Research. 2023;24:35.
- Aggarwal A, et al. J Cutan Aesthet Surg. 2020;13(4):265–274
- NHS. Post-herpetic neuralgia, 2021. Available at: https://www.nhs.uk/conditions/post-herpetic-neuralgia/treatment/. Accessed March 2025.
- Yanni EA, et al. BMJ Open. 2018;8:e02028.
- Kovac M, et al. Vaccine. 2018;14;36(12):1537–1541.
- Andrews N, et al. BMJ Open. 2020;10:e037458.
- Tan PS, et al. BMJ Open. 2023;13(3):e058705.
- NHS. Shingles. Available at: https://www.nhs.uk/conditions/shingles/. Accessed March 2025.
- NICE CKS. Shingles Management. Available at: https://cks.nice.org.uk/topics/shingles/management/management/. Accessed March 2025.
- Acosta EP, Balfour HH Jr. Antimicrob Agents Chemother. 2001;45(10):2771–2774.
- NHS Inform. Shingles. Available at: https://www.nhsinform.scot/illnesses-and-conditions/infections-and-poisoning/shingles. Accessed March 2025.
- Harvard Health Publishing. Shingles (herpes zoster). Available at: https://www.health.harvard.edu/a_to_z/shingles-herpes-zoster-a-to-z. Accessed March 2025.
March 2025 | PM-GB-AVU-WCNT-230003 (V6.0)
For the SHINGRIX® (herpes zoster vaccine, recombinant, adjuvanted) prescribing information, click here.










