Shingles Vaccine Case Study: How a GP Federation Increased Vaccination Uptake
July 2024
Read time: 8 minutes
Topic tags: Bury GP federation, shingles vaccine uptake
Return to Educational ResourcesAdverse events reporting and prescribing information can be found at the bottom of the page.
Healthcare professionals have been consulted by GSK and received honorarium.
Delve into the successful approach adopted by a GP Federation
Do you know your practice’s shingles vaccination uptake rate?
Read on to discover how the Bury GP Federation transformed their practice with achievable, simple steps that had a considerable impact on vaccine uptake, and get top tips that you can take away and apply to your clinical practice. Bury's lower uptake provided an opportunity to identify, understand and address barriers to implementation. GSK partnered with Bury GP Federation through a collaborative working project.
The state of play
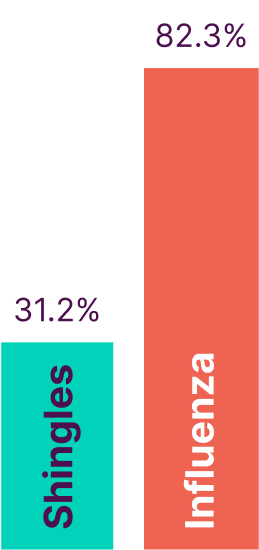
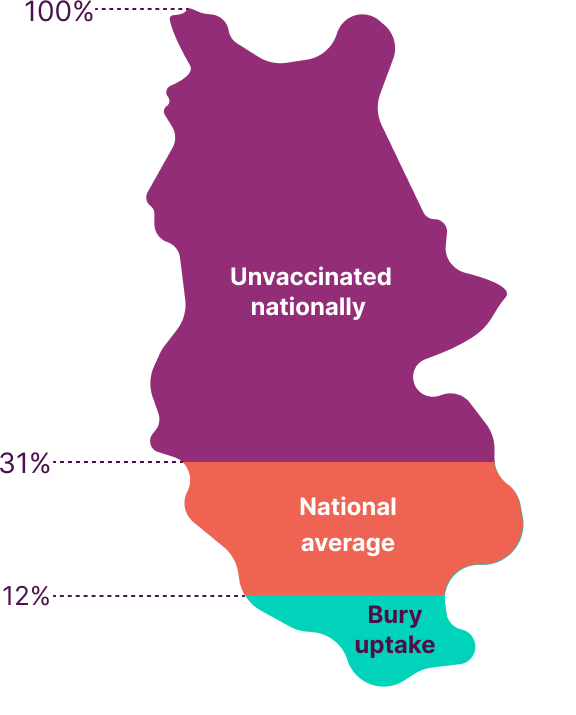
The Shingles NIP aims to reduce the incidence and severity of shingles in older people. However, low uptake in many areas of the country leaves many patients vulnerable to this vaccine-preventable disease.
This low uptake also negatively impacts resource utilisation through follow-up appointments and management of shingles cases and its associated complications.3
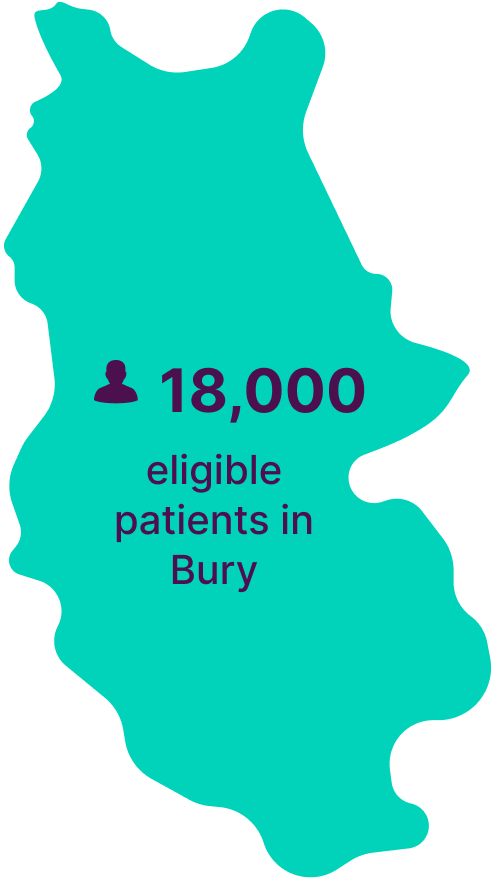
Bury, situated within the Greater Manchester Integrated Care Board, encompasses 25 GP practices with 210,000 patients, 18,000 of whom meet the Shingles NIP eligibility criteria (pre-1st September 2023 update).
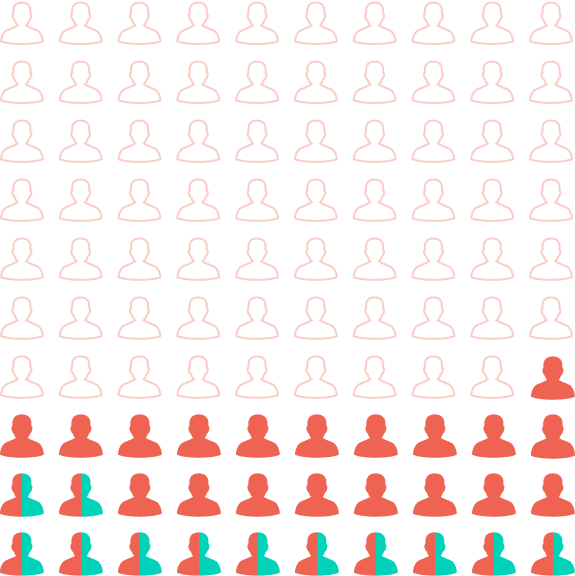
![]() 12% uptake in Bury
12% uptake in Bury
![]() 31% national average
31% national average
![]() Unvaccinated
Unvaccinated
Approach – A plan in three stages
In the pursuit of optimising existing resources and systems to enhance vaccine uptake, a strategic roadmap was devised, comprising three crucial stages: ‘Understanding’, 'Solutions’, and 'Actions’.
The initial ‘Understanding’ phase analysed and identified the current challenges and barriers to vaccine uptake. The ‘Solutions’ stage required collaborative efforts to implement targeted interventions, optimising existing resources and systems. The final stage, ‘Actions’, saw the execution of these solutions, followed by a rigorous assessment of their impact.
As you read through, think about how you might use something similar in your practice.
 Hover on the cards to see more
Hover on the cards to see more
Approach stage 1: Understanding
Stage 1 identified key barriers and opportunities for shingles vaccination in the Bury GP Federation. Four key themes that contributed to low practice uptake emerged.
How does your practice compare to the practices in Bury GP Federation?
Use the interactive buttons to explore and understand the challenges and behaviours that affect practice performance.
Approach stage 2: Solutions
Practices were segmented into three groups based on current uptake, capability, and support needs. Use the interactive buttons below to explore these groups.
Key takeaway
Every practice is unique. Therefore, understanding the challenges faced by yours is important to help you make simple improvements that can make a big difference.
You can ask yourself some key questions: Do you know how many eligible patients are still unvaccinated? How proactive and structured is your call/recall system? How are you driving patient engagement?
Find time to proactively think about the challenges faced by your practice to help identify the right approach for you and your team to address them.
Approach stage 3: Actions
Shown below are the four key themes identified as contributing factors to low practice uptake that could be optimised to improve vaccine rates.
Use the interactive buttons to explore the implemented solutions devised to address these challenges.
Results: Impact
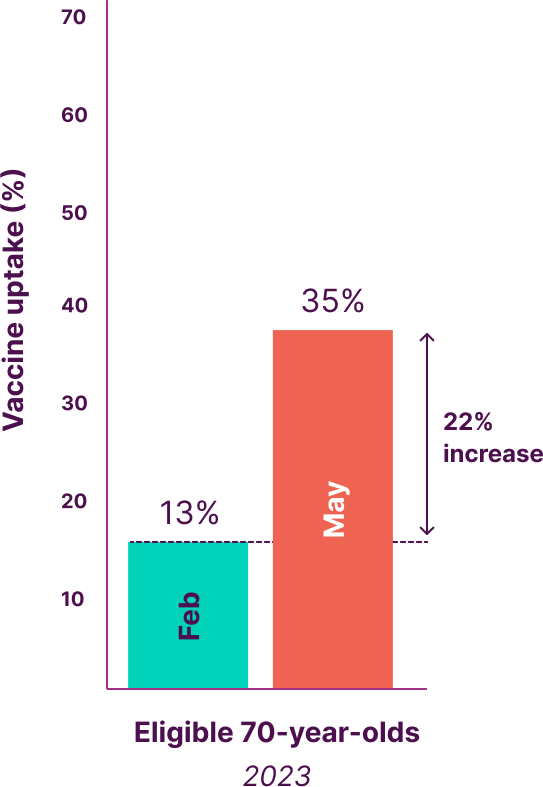
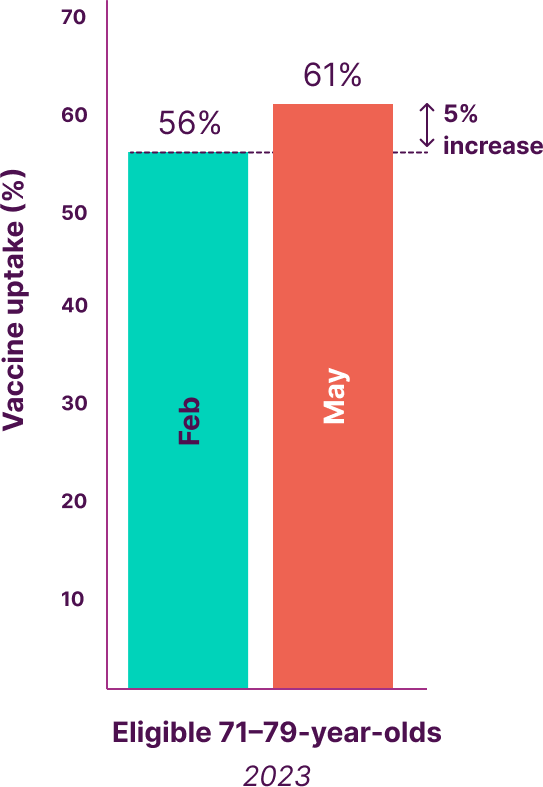
In a remarkable achievement, Bury elevated shingles vaccination uptake by an impressive 21% within 4 months, by using only existing resources. Strategic optimisation, including automated appointment invites, freed up administrative time for other tasks.
Key actionable stepsWhat can be learnt from this, and implemented in more practices?
The project’s initiatives yielded substantial benefits for practices within the Bury GP Federation and its patients.
There is an opportunity to use this as a blueprint for working collaboratively to implement effective shingles vaccination programmes across a PCN or GP Federation, or to take many of these learnings and apply them directly to your practice.
Key lessons from this project included:
- Clinics with a range of times and dates across all areas boosted vaccination uptake. Through a reorganisation of existing clinical resource, flexible out of hours appointments and advanced online booking was used, which increased vaccination appointments
- Practices with online platforms or appointment booking links empowered patients to self-book, freeing phone lines and reducing administrative resource that was originally required to invite and book patients in for their shingles vaccine appointment
- Each practice had a designated Immunisation Lead who worked with a project manager to plan and implement practice-level solutions. The Immunisation Lead also ensured there was a clear understanding and awareness among staff of the importance of the shingles vaccination
- Each practice had a single accountable individual who ordered vaccine stock through ImmForm. This meant there was a clear understanding of who oversaw their clinics vaccine resources and helped to avoid hesitancy
- Addressing IT and EHR knowledge gaps through regular training and support improved staff capability. Nurses now seamlessly update patient EMIS records during clinics, streamlining processes and elevating overall efficiency
Shingles vaccine uptake (%)
This collaborative working project included Bury GP Federation (which is composed of 3 Primary Care Networks (PCN)) and a standalone PCN. The graph below displays the vaccination coverage rate for eligible 70-year-olds and eligible 71-79-year-olds, when the project commenced in February 2023 and upon completion in May 2023.
Across all 4 PCN’s, the total number of eligible patients was as follows:
- 1,929 Eligible 70-year-olds, February 2023
- 15,969 Eligible 71-79-year-olds, February 2023
- 1,901 Eligible 70-year-olds, May 2023
- 15,855 Eligible 71-79-year-olds, May 2023
*Standalone PCN within the borough of Bury.
Outcomes summary
The Bury GP Federation showed a considerable improvement in shingles vaccination uptake. This increase highlights the importance of regularly reviewing how your practice implements NIPs, and the effectiveness of strategically optimising existing resources tailored for a practice’s needs and requirements.
The success of this shingles vaccine case study shows the potential for targeted resource utilisation to drive shingles vaccine uptake nationally.
- The first step was to identify the main barriers to shingles vaccination uptake and find ways to address them
- By examining these barriers, the team discovered opportunities to better use existing facilities, team members, and services, without the need for a complete overhaul or hiring additional clinical staff
- By taking action on these opportunities, Bury, which previously had a significantly lower shingles vaccination uptake compared to the national average, managed to considerably boost shingles vaccination rates in all practices
- This case demonstrates that even simple changes can have a big impact on the delivery of shingles vaccinations, improving the overall uptake and helping to protect more people
What could you do to optimise your practice?

Delivering the Shingles National Immunisation Programme in your practice.
Explore our handy infographic filled with practical advice and guidance, and a downloadable checklist detailing key steps for implementation.

Immunisation Leadership in Practice
What do we mean when we talk about the role of an Immunisation Lead? In this article we look at how a practice might approach immunisation leadership, and the key roles and responsibilities of an Immunisation Lead.
References
- UKHSA Seasonal influenza vaccine uptake in GP patients: Winter season 2021 to 2022. Available at: https://www.gov.uk/government/statistics/seasonal-influenza-vaccine-uptake-in-gp-patients-winter-season-2021-to-2022. Accessed July 2024.
- UKHSA Shingles vaccine coverage (England): Annual report of the financial year 2021 to 2022. Available at: https://www.gov.uk/government/publications/herpes-zoster-shingles-immunisation-programme-2021-to-2022-evaluation-reports/shingles-vaccine-coverage-england-annual-report-of-the-financial-year-2021-to-2022. Accessed July 2024.
- Andrews N, et al. BMJ Open. 2020;10(7):e037458.
March 2025 | PM-GB-AVU-WCNT-230012 (V2.0)
For the SHINGRIX® (herpes zoster vaccine, recombinant, adjuvanted) prescribing information, click here.